







Privileging 101 - Introduction to Privileges: Back to Basics - Physicians

As a Medical Services Professional (MSP), your main job is to keep patients safe. To protect patients, you must adhere to complex and lengthy credentialing and privileging processes to screen providers, verify their ability to practice, and determine which procedures and services they're competent to deliver. This is a complicated and involved process that cannot be phoned in; HealthStream understands and wants to help. That's why we created our webinar series, Privileging 101, which provides all the information you need to become a privileging pro.
In this series, we cover it all, from basic education on the history and fundamentals of clinical privileging to how to navigate all the regulatory and legal aspects involved. It's an ideal fit for MSPs new to the field of privileging and any pros looking to gain additional knowledge of privileging processes.
In part one of the series, Privileging 101 - Introduction to Privileges: Back to Basics - Physicians, we explain why privileging exists and provide an overview of the journey physicians must complete before they can apply for privileges. Read on for the highlights of this session.
Why privileging exists
Privileging is here for protection. It functions to protect patients, the organization, and the provider. It also helps MSPs meet regulatory requirements for accreditation standards. Privileging is the most effective mechanism for ensuring quality delivery of excellent care treatment within an organization, which is why it is such a vital component of what MSPs do. That is also why it is so critical that MSPs are able to effectively privilege providers as it has an effect on the entire medical system.
Privileging involves four basic steps:
- The organization determines the scope of services and procedures it will offer and support.
- Then they determine the minimum criteria or qualifications required for those services.
- The organization then evaluates whether the applicant meets the requirements.
- Finally, the organization monitors privileges granted to providers to ensure current competency.
How physicians come to be
There's a whole lot of training that needs to happen before someone can become a physician. Once a person completes pre-med and graduates from medical school, they can apply for a residency in a particular specialty, and depending on the specialty, it can take anywhere between three to seven years to complete.
Physicians can train to be various kinds of doctors, some examples include:
- MD: A Medical Doctor who treats disorders and injuries by using methods aimed to counteract symptoms to promote healing.
- DO: A Doctor of Osteopathic Medicine is a fully licensed physician who practices in all areas of medicine with an emphasis on a whole-person approach to treatment and care.
- DDS: A Doctor of Dental Surgery provides dental care, and has the same level of licensure as a DO.
- DPM: Stands for a Doctor of Podiatric Medicine, working with a focus on the lower extremities, mainly feet, and ankles.
If a physician completes their residency and decides to further their education, that's called a fellowship. There are a variety of fellowship programs with different areas of focus, like pediatric and vascular surgery, surgical critical care, and complex general surgical oncology. Once physicians have their training in place, licensure is necessary.
What professional licensure entails
Once a physician has completed their residency, they must obtain a medical license before they can practice. Licenses are specific to the respective state or territory they will be practicing in. Every state has specific requirements for when a resident position may begin the application process to obtain their state license. To obtain licensure, all physicians must have:
- Graduated from an approved medical school
- Completed an approved residency
- Passed a licensing examination
There's a lot more to the process, but those three steps outline the basic timeline of events as required by the Federation of State Medical boards or FSMB. They represent the state medical and osteopathic regulatory boards, commonly referred to as state medical boards within the United States, its territories, and the District of Columbia. They support the USA's state medical boards in licensing, disciplining, and regulating physicians and other healthcare professionals.
How board certifications come into play
Board certifications are interesting as they are not mandatory, but they are definitely considered an essential component in determining a physician's expertise and experience in a particular field of medicine. Board certification indicates advanced knowledge, training, and skills and helps patients identify qualified specialists. There are five steps required of a physician to obtain board certification:
- They must complete four years of medical education in college or university.
- They have to earn a medical degree from a qualified school.
- They have to complete 3-7 years of full-time experience in residency training by a semi-accredited program.
- They have to provide letters of attestation from a program director.
- They have to obtain an unrestricted medical license to practice within the United States or Canada.
There are some specialty boards that may vary on these specific requirements, but these are a good starter list to work off of. You can find more in-depth information on their individual board websites. In fact, you'll also find specific guidelines for recertification, much of which will be helpful when it comes to developing the criteria and qualifications expected for granting privileges.
There are three organizations that serve as the trusted authority for board certification for physicians:
- The American Board of Medical Specialties (ABMS): They have been around for over 85 years, and have 24 member boards with 40 specialty areas in 88 sub-specialty areas.
- The American Osteopathic Association: They were founded in 1897, and represent 16 specialty boards with 27 primary board certifications in 48 sub-specialty certifications.
- The Royal College of Physicians and Surgeons of Canada: They were established in 1929, and they recognize over 100 specialties, subspecialties, and special programs.
There are three different kinds of board certifications a physician can obtain:
- Primary Certification
- Granted to physicians for successfully completing and maintaining requirements for their primary specialty.
- Subspecialty Certification
- Granted to physicians for successfully completing and maintaining requirements for their primary specialty.
- Requires completion of additional Accreditation Council for Graduate Medical Education (ACGME) accredited fellowship training for at least one year.
- Focused Practice Designation
- Granted to a physician who demonstrates additional expertise and continued focus in a particular area of specialty or subspecialty.
What are ACGME core competencies
Core competency represents a provider's ability to do a particular activity to a prescribed standard or with a desired outcome based on knowledge, education, training, traits, skills, and abilities. It is a principle of professional practice, identifying the ability of a provider to administer safe and reliable care on a consistent basis.
As of July 2022, the Accreditation Council for Graduate Medical Education (ACGME) instructed all residency programs to require their residents to demonstrate competency in six core areas:
- Patient care and procedural skills
- Interpersonal and communication skills
- Medical knowledge
- Professionalism
- Practice-based learning
- Systems-based practice
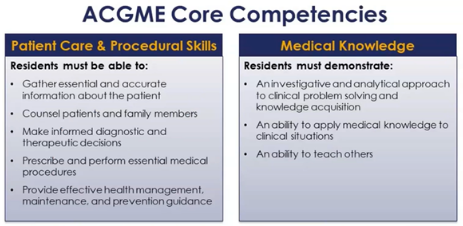
Each of the six core competencies has specific assessment methods, most of which are included in the privileging process whether through peer reference simulation labs, case logs, observation or physician feedback. The overarching goal is to produce physicians that can be entrusted to provide the highest level of quality care for the benefit of the public.
How specialty societies play a part
Specialty societies serve to promote, advance, and educate their members through the development and publication of evidence-based clinical practice guidelines, position papers, medical consensus documents, journals or publications, as well as conferences or seminars. Simply put, they support physicians by continuously contributing to quality improvement efforts primarily through education via a variety of outreach efforts. This is one way that physicians can come together to create shared common standards for different treatments.
How Medical Staff Governance works
When it comes to medical staff structure, the governing board is always at the top. They are the highest level of governance in an organization, accountable for the quality and safety of care delivered by the organization.
In a multi-hospital system with a unified staff, the governing board delegates responsibility and accountability to the medical staff and administration for the quality of care provided by providers who have been granted privileges within the organization. They will monitor processes and procedures including credentialing, privileging, and peer review.
In a multi-hospital system with individual medical staff, there will be a system governing board at the very top, to which each of the individual hospitals' governing board reports. This happens when hospitals have their own separate CMS, Medicare, or CCN number. In terms of CMS requirements, only the hospital's governing body has the authority to grant practitioners privileges to provide care in the hospital.
In summary
That's a lot of info, isn't it? And this is just an overview of the first session, Privileging 101 - Introduction to Privileges: Back to Basics - Physicians, in our extensive series on privileging. If you found this helpful, then we definitely recommend you check out the entire Privileging 101 series for yourself, and as always, feel free to reach out with any questions.
