







Increased Regulations Drive the Need for Standardized Data and Automation

The complexities around credentialing, privileging, and provider enrollmentare increasing every day. Over the past year, the surge in emergency patientsassociated with COVID19 and the skyrocketing demand for telehealth services,have made it abundantly clear that rapidly onboarding, credentialing, privileging,and enrolling providers in payer plans is more critical than ever. Accelerating thisprocess is no easy feat given the fact that every payer and regulatory agency hasits own unique set of requirements.
In the past, it was possible to manage credentialing, privileging, and providerenrollment data with limited resources and with separate systems and processes.Today, payers and regulatory agencies expect healthcare organizations to gofurther - driving a greater demand for data integrity.
According to the American Hospital Association,"Health systems, hospitalsand PAC providers must comply with 629 discrete regulatory requirementsacross nine domains."
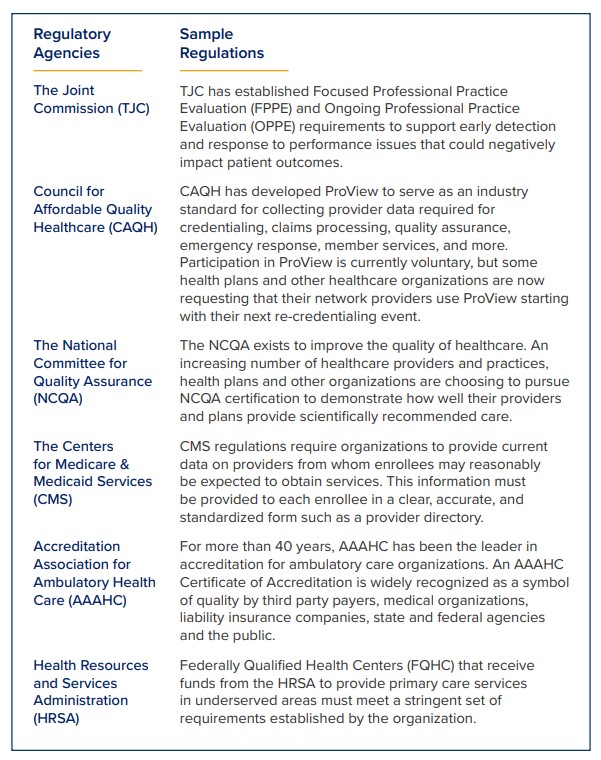
Tracking and researching regulatory requirements across various bodies andnegotiating contracts with individual payers can eat up a lot of time. Inaccuraciescan lead to costly compliance issues. The good news is that:
- VerityStream does this research for you and delivers the most up to date standardized data and content on an ongoing basis via our CredentialStream solution.
- We've designed multiple methods (depending on your state) to get you started on standardizing and migrating your data.
Standardizing Your Data
Standardizing your data collection of the following information can save countlesshours and dollars for your organization:
- Proof of Identity
- Education and Training
- Military Service
- Professional Licensure
- DEA Registration and State DPS and CDS Certifications
- Board Certification
- Affiliation and Work History
- Criminal Background Disclosure
- Sanctions Disclosure
- Health Status
- National Practitioner Data Bank (NPDB)
- Malpractice Insurance
- Professional & Peer References
This can certainly be a daunting task. The process involves making sure that eachdata type has consistent content and a similar format. If there is inconsistencyacross your data fields for each provider, that data will not be easily reportableor useful. And it definitely won't make automating your entire provider lifecyclepossible.
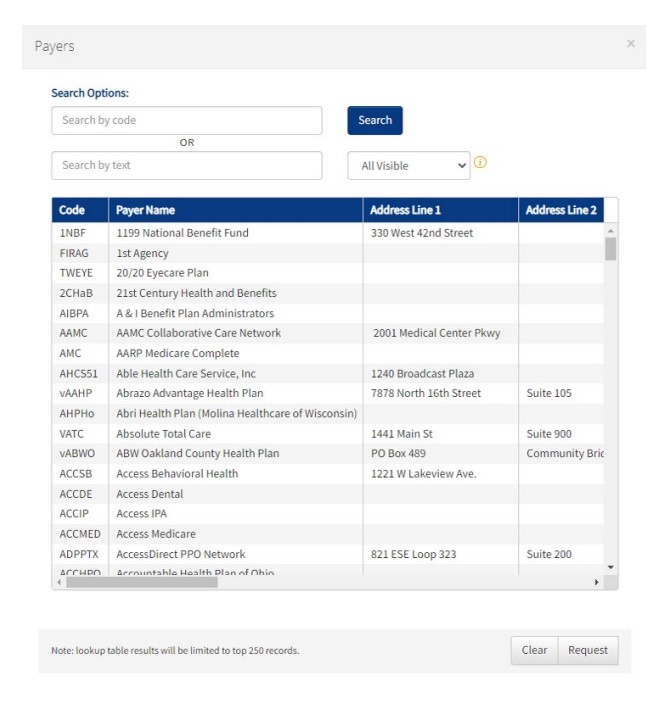
- CredentialStream's vSource shared data tables are validated, integrated, and continuously updated including facilities, schools, payers, license boards, and health status including the COVID-19 vaccine. These data tables have been built around regulatory requirements.
- VerityStream offers multiple solutions for standardizing and migrating your data to CredentialStream that fit your unique state, whether you have millions of lines of data, or a practice of 25 providers. Learn more about data migration options here.
Making Your Data Work for You
CredentialStream's VerityStream Validated Providers (VVP) offers pre-populated,validated provider data that reduces the overhead required for repetitiveresearch tasks and expedites turnaround times. With VVP, a single providerrecord can now be used to support all credentialing, privileging and enrollmentoperations, removing the need for multiple spreadsheets and checklists. Thisnot only improves data integrity, but also speeds up your processes. And, morestreamlined workflow management promotes compliance through the generationof reminders related to requirements from the growing number of regulatoryagencies overseeing your performance.
Bottomline
Migrating to CredentialStream offers a path to transforming your credentialing,privileging, and enrollment operations with standardized, pre-validated data toaccelerate onboarding times, improve the provider experience, and meet thedemands imposed by ever-changing healthcare regulations.
Contact your VerityStream Sales Representative to learn more about our datastandardization and migration paths.
</pthankfully,>
